Hepatitis B + D = BAD

HEPATITIS B can produce four states:
1) acute with resolution
2) chronic hepatitis
3) fulminant hepatitis with massive liver necrosis
4) backdrop for hepatitis D viral infx
HEPATITIS B
--a hardy virus that "can live for 2 weeks on a dry coffee cup" according to Denny
--formerly known as "serum hepatitis", or the Dane particle
--can withstand extreme temperatures
--INCIDENCE AND RISKS
--strongly associated with the development of HEPATOCELLULAR CARCINOMA
--2 billion individuals living today have been infected with HBV at some point
--in the US there are approximately 185,000 new inections/year
--INCUBATION: 4-26 weeks or 6 weeks to 6 months depending on source
--TRANSMISSION: blood and body fluids: transfusions, dialysis, needles, sex, mother to infant at birth? or before?, semen, vaginal fluids, tears, saliva
--vertical transmission is common in Africa and SE Asia, infants become carriers, may cross placenta and infect fetus before birth
--20-60% of births to infected mothers result in transmission
--in 1/3 of pts the source of infx is unknown
--cocaine use probably favors transmission
--contaminated needle stick risk of infection is abou 45%!!
--IMMUNIZATION is offered for healthcare workers and is a series of three shots with months between them. 30-50% of the immunized lose antibodies in 7 years and require a booster. Some are immune for life. Get an anti-HBs Abs titer to be sure.
--HBV remins in the blood up to and during active episodes of acute and chronic hep
--HBV is present in all physiologic and pathologic body fluids EXCEPT the stool
--no evidence of transmission by kissing
--in the west, newborns are vaccinated for hep B at birth, long before the infant's immune system is developed enough to mount an appropriate response to the vaccine. Twould be much better to hold off on this vaccination until the infant is at least 18 months of age.
--pregnant mothers are tested twice for hep B during the pregnancy, 6 months apart, so that if she was newly infected at the time of the first testing the antibodies will show up for the second testing
CHRONIC HEP B
--5-10%of acute cases become chronic
--carriers have actively replicating virus and are a source of infection
--worldwide there are an estimated 350 million carriers
--75% of all chronic carriers live in Asia and the Western Pacific rim
--prevalence of chronic hep B varies from over 8% in Africa, Asia and the Western Pacific, to 2-7% in Southern and Eastern Europe, to under 2% in Western Europe, North America, and Australia.

HEP B TESTING
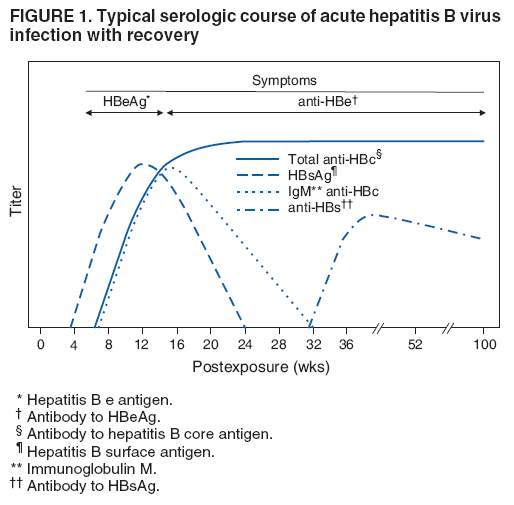
--look for: HBsAg (first antigen), HBeAg (replicative antigen), Anti-HBc (immune response, IgM and total M&G), Anti-HBe (good prognosis for resolution), Anti-HBs, and HBV DNA
--outer envelope contains Hep B surface antigen: HbsAg which is detectable in serum
--viral center contains double stranded DNA and DNA polymerase
--2 "core" antigens surround the viral genome: HBcAg and HBeAg (the "e" is for "exportable")
--HBeAg is detectable in serum (c is not bcs surrounded by HBsAg)
--FIRST indicator of HBV infx: HBsAg, the surface antigen, appears 27-41 days after exposure and 7-26 days before biochemical abnormalities, peaks as ALT rises and may persist during acute illness. Disappears 12-20 weeks after onset of Sx in 90-95% of cases. If HBsAg persists more than 6 MONTHS it is defined as a CHRONIC HBV infection.
--HBsAg is used as a diagnostic screen for HBV infection however 10% may present with illness after the surface antigen has cleared. TO BE SURE test for anti-HBc IgM, the initial antibody to the core antigen. The infection may clear or may become chronic from a + at this stage.
--if HBeAg is present, the pt is highly contagious due to active HBV replication. HBeAg appears within 1 wek after HBsAg. In acute cases that resolve, HBeAg is present for 3-6 weeks then disappears before HBsAg. Use to determine RESOLUTION of infection. If it persists over 20 weeks suggestive of progression to chronic HBV with active viral replication.
--Anti-HBc IgM appears 2-4 weeks after HBsAg appears, and is replaced with IgG in about 6 months. Anti-HBcAb IgG remains for life but does not correlate with resolution of infection, as it will be present in individuals who have chronic infection as well as those that resolve.
--Anti-HBc present in absence of HBsAg and anti-HBs: confirms recent acute (2-16 weeks)
--Anti-HBe appears only if HBeAg disappears, and remains detectable for years. Indicates decreasing infectivity and good prognosis for resolution of acutes.
--90-95% recover from acutes, confirmed by presence of Abs w/o HBsAg, conferring immunity
--appearance of antibodies may tak weeks/months after HBsAg has disappeared and ALT HAS NORMALIZED
--the gap between the disappearance of HBsAg and appearance of anti-HBsAb (2-6 weeks) is known as the "core window" or serologic gap.
--TO CHECK EFFECTIVENESS OF HEP A IMMUNIZATION: test Ani-HBsAb
--30-50% loose antibodies in 7 years after immunization and require a booster. I got the shots when I worked ski patrol in the early 90's and still had ABs when tested in 2006.
--THE MOST SENSITIVE AND SPECIFIC ASSAY FOR EARLY EVALUATION IS: PCR. Measures HBV replication even when HBeAg is not detectable. This is how you measure "viral load". People with HBV DNA > 200 pg/mL are less likely to respond to interferon therapy.


HEPATITIS D
--the "Delta Agent"
--HDV is an RNA virus that depends on HBV for expression and replication
--superinfection wth D and B is much more severe illness than B alone
--prevalence in US is 1-10% of HbSAg carriers
--HDV hepatitis is often severe with relatively high mortality in acute dz
--cirrhosis is a frequent development in chronic disease
--HBV more virulent in presence of Hep D-->fulminant liver necrosis and death may occur
--a unique RNA virus that is replication defective
--causes infx only when encapsulated by HBsAg
--distinct from HBV but dependent on genetic info from HBV for multiplication
--causes dz only in presence of HBV
--TRANS: needles and sex
--two ways delta hepatitis arises: acute co-infection when exposed to serum containing both HDV and HBV, or superinfection of D after a pt is already infected with HBV
--INCIDENCE: rare in US, except among IV drug abuses and blood product users: hemophiliacs
--more in Mediterranean, Middle East and northern Africa
TESTING FOR HDV
--Dx: find anti-HDV in pt with HBsAg positive hepatitis
--anti-HDV is not performed unless HBV infx is confirmed
--COINFECTION: simultaneous acute infection of both B and D, usudt blood products. HBsAg and anti-HBc IgM indicate acute HBV, plus anti-HDV IgM documents acute HDV
--SUPERINFECTION: acute HDV in chronic HBV carrier (much more common), HBsAg and Anti-HDV IgM, ABSENCE of Anti-HBc IgM.
--PCR--RNA HDV serum test to confirm either
HEPATOCELLULAR CARCINOMA
--most frequent primary liver cancer: malignant
--aka hepatoma
--strong assocation with hep B infx
--most common visceral tumor
--often arises in setting of cirrhosis
--infants who contract HBV at birth have 200 fold risk of this CA
--in the US chronic alcoholism is most common cause of this CA
--greenish yellow hue
--elevated serum alpha-fetoprotein -- follow!
--mass may obstruct biliary tract-->elevated ALP
--markers: CA 19-9 and CA-50 are usu positive in cases of cholangiocarcinoma while often negative in cases of hepatocellular carcinoma